Day in and day out, the University of Chicago Medicine campus is teeming with activity, as scores of physicians, nurses and other hospital employees provide care and service to patients. Part of that care involves ordering tests for a variety of reasons, such as diagnosing a disorder, evaluating the severity of a disease and monitoring patients’ responses to treatments, among others.
Patients and clinicians at UChicago Medicine have the benefit of a unique, state-of-the-art facility on the medical campus, one that sits below six floors of the Bernard Mitchell Hospital. There, inside a 7-foot-thick concrete vault, a machine called a cyclotron can produce radioactive isotopes that can help physicians identify diseases or other health conditions, as well as track their progression.
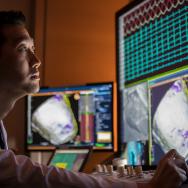
The University of Chicago Cyclotron Facility lies on the other side of an unassuming door in the Medical Center’s underground tunnels. Opened in 2017, the facility is run by a staff of three, including program director Richard Freifelder.
Despite its small team, the facility produces many radioactive drugs used not only by research and clinical faculty at UChicago, but by those at other institutions in Illinois and surrounding states. This is because UChicago Medicine is the only academic health system in Illinois with an operational cyclotron.
The cyclotron is giving current doctors and patients access to care and diagnoses, but also spurring new lines of inquiry and research that can lead to new understanding of and treatments for disease.
Why do doctors need radioactive isotopes?
Multiple types of medicine use radioactive isotopes. These isotopes have the special ability to light up on scans, so doctors can easily see and track their progression through the body. For example, a PET scan can show doctors if a particular area of the body is growing abnormally fast—which could, for example, indicate a tumor. It can also give doctors and scientists a look at processes that are hard to see otherwise, such as how plaque accumulates in the brains of Alzheimers’ patients.
The isotopes are short-lived, so they then decay quickly inside the body. This field is called nuclear medicine.
What is a cyclotron?
A cyclotron is a machine that accelerates a particle along a spiral path. The particle’s energy increases as it circulates through the machine. Once it has gained enough energy, the particle hits a target and a nuclear reaction occurs, producing a radioactive element of interest.
“The main reaction we use is a proton on an Oxygen-18 target,” said Freifelder. “When the proton bombards the Oxygen-18, which is stable, it is converted into Fluorine-18, which is a radioactive isotope.”
Once the Fluorine-18 (F18) is produced, it is captured for synthesizing into a drug. Other radioactive elements, such as Carbon-11 and Oxygen-15, can also be produced in the cyclotron. “Each of these is made by some particle bombarding an appropriately-selected target to create a short-lived radioactive isotope,” explained Freifelder.
A radioactive isotope, or radioisotope, is an unstable version of an element, meaning that it releases its energy over time via a process called radioactive decay, usually by converting to electromagnetic waves or new particles. F18 primarily decays into particles called positrons. This is what the “positron” in a Positron Emission Tomography (PET) scan refers to.
How does PET work?
A PET scan creates images of the body, allowing a radiologist to evaluate abnormalities in processes such as metabolism, blood flow or chemical absorption. The images are taken using a special camera that captures gamma rays—electromagnetic radiation that is invisible to the naked eye.
The gamma rays are produced inside the body, through the interaction of a specialized drug and naturally occurring particles within the body’s tissues.
The drug, given to a patient before their scan, acts as a sort of Trojan horse. For instance, the drug may look to the body like glucose, in which case a region that needs energy, like a growing tumor, will readily use it. But the drug isn’t really glucose. It’s a mimic, and it contains a radioactive isotope that emits positrons. When these positrons, or anti-electrons, interact with electrons in the body, they annihilate, releasing gamma rays. So, as the tumor is trying to utilize the drug, it is also enabling physicians to see, study and ultimately, attempt to eliminate the tumor.
The UChicago Cyclotron Facility produces both the radioactive isotope, which decays via positron emission, thus creating gamma rays for PET imaging, and the drug that contains the isotope. Once the isotope is produced in the cyclotron, it is transported to a cleanroom, containing a hot cell, a chamber shielded by three inches of lead. There, radiochemist Mohammed Parvez Bhuiyan and radiochemistry specialist and cyclotron operator Anna Kucharski synthesize the drug.
While the radioisotope is a critical component of the process, Freifelder noted that “the specificity of these drugs is dependent on the particular chemistry. The radioactive tag is then just carried along.”
Why have a cyclotron at UChicago?
The moment F18 or any other radioisotope is produced, it begins decaying. After about two hours, half of it has emitted its positrons and decayed back to stable Oxygen-18. After about 10 hours, there is almost no F18 left. This means that the drug synthesis and subsequent PET scan must both occur within a few hours after the F18 is produced from the cyclotron. The drugs must be produced daily for that day’s usage and cannot be stored.
Other radioisotopes and radiopharmaceuticals can have even faster decay rates. The faster the rate, the sooner imaging must take place, limiting the delivery radius for the drugs. Moreover, while F18 and some of the PET drugs that use it might be available from a nearby privately-owned, commercial cyclotron, less common radioisotopes and drugs are often too difficult or expensive to produce or cannot be included in the commercial operation’s schedule and therefore are not readily accessible.
The UChicago Cyclotron Facility provides a way for researchers and clinicians to not only obtain well-known radioactive drugs conveniently and economically, but to collaborate on producing and utilizing less common or even completely novel ones.
For these reasons, the 2017 opening of the facility has reinvigorated radio-imaging research at UChicago and surrounding institutions. Before this, UChicago had not had a cyclotron since 1998, when the original machine (then housed in the subbasement of the Frank McLean Institute) was decommissioned. That machine, which had been operating since 1968, was an integral part of UChicago’s history at the leading edge of nuclear medicine research. Faculty at that time, including Katherine Lathrop, Lester Skaggs and Robert Beck, utilized this new technology to pioneer radiation-based imaging and treatments.
From 1998 to 2017, however, researchers at UChicago and surrounding institutions were without a local facility and dedicated team to assist in producing radioisotopes and radiopharmaceuticals for use in basic research, clinical studies or patient imaging.
“Some drugs were just not available,” said Freifelder. “Some you could get out of a commercial vendor, but you’d be paying a lot. It was limited and it was very expensive. Now, it’s opening up.”
This change was driven in part by the vision of Chin-Tu Chen, the facility’s scientific director, who earned support from the Biological Sciences Division’s Dean’s Office, the University of Chicago Comprehensive Cancer Center, the Duchossois Foundation, the O’Connor Foundation, and the Ludwig Foundation.
What is the facility working on now?
In addition to producing well-established radioactive drugs, the Cyclotron Facility is currently collaborating with researchers at UChicago and nearby institutions (including Rush University Medical Center, Advocate Health Care, and the University of Illinois at Chicago) and companies to make less-common drugs and develop new ones. For example, Freifelder’s team is producing drugs that bind specifically to tau proteins and amyloid-beta peptides—molecules that aggregate in the brains of patients with Alzheimer’s disease. This enables researchers and clinicians to visualize the distribution of these proteins in humans, in vivo.
“We have been making the tau agent for over two months,” said Freifelder. “It is currently being used in clinical trials in humans.” The amyloid agent is undergoing its final validation runs in the facility, and Freifelder expects it to be ready to ship in a couple of months.
Freifelder’s team is also producing a drug to assist in imaging brains suffering from traumatic injury, based on an original request from Northwestern University. Now, researchers at UChicago are also utilizing the drug.
“We are collaborative,” said Freifelder. “This means supporting our sister institutions in the area.” It also means working closely with researchers to develop new methods and products.
The ability to have these conversations is itself a perk of having a cyclotron on campus. “It’s an educational process,” Freifelder said. This process enables faculty to develop their ideas alongside Facility experts, increasing the probability of successful research and eventual clinical trials and treatments.
This commitment to collaboration has helped the UChicago Cyclotron Facility establish itself as an integral part of research efforts at the University and in the surrounding community. With plans to further grow and innovate, the Facility is sure to remain humming away under Mitchell Hospital for years to come.
Click here to learn more about the Cyclotron Facility and the compounds it currently produces.
—Adapted from an article first published by the Biological Sciences Division.