Even after decades of research, cancer remains difficult to treat, in part because of its ability to evade the body’s natural defenses found in the immune system.
Immunotherapy, which stimulates the body’s immune system to find and attack cancer and other diseases, has offered a new avenue for treatment. Despite successes, only a fraction of cancer patients responds to these therapies, and many experience adverse side effects, including pain and inflammation.
Researchers in the Institute for Molecular Engineering at the University of Chicago have developed a new way to target immunotherapies and deliver them directly to tumors, helping to both reduce side effects and make the therapies more effective in treating cancer.
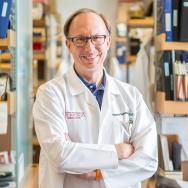
“Immunotherapies show great promise in treating cancer, but they are often toxic and not as effective within the body,” said Jeffrey Hubbell, the Eugene Bell Professor in Tissue Engineering who co-authored the research, published April 10 in the journal Science Translational Medicine. “If we can target their delivery and help more patients respond to immunotherapy, it would really change the story of cancer treatment and give patients more treatment options.”
Improving efficacy of immunotherapy
The immune system has a poor track record of fighting off cancer because it uses checkpoints—molecules on immune cells that need to be activated to start an immune response—to determine if a cell is a foreign invader.
Cancer cells can hijack these checkpoints to avoid detection by the immune system. Immunotherapies are designed to circumvent that outcome, and doctors often use one or a combination of these therapies to treat some cancers.
One therapy, called checkpoint inhibitors (CPIs), works by blocking proteins and allowing immune cells to find and attack cancer. Another, called interleukin (IL)-2, a protein made by white blood cells that increases the growth of immune cells, works by stimulating the immune system to attack cancer.
Though these therapies have helped treat cancer in many patients, they can overstimulate the immune system, leading to liver toxicity and inflammation throughout the body.
Targeting collagen
Hubbell and his collaborators, including Melody Swartz, the William B. Ogden Professor and co-author of the research, and postdoctoral fellow Jun Ishihara, wanted to find a new way to deliver these drugs specifically to the tumors they were meant to target.
While other researchers have taken similar approaches and developed systems that target a specific tumor protein or the tumor’s DNA, the University of Chicago researchers decided to take a unique approach: targeting collagen.
Collagen is one of the most abundant proteins in the body. It is especially abundant in tumors. Researchers hypothesized that if they could find a way to deliver immunotherapies directly to the collagen in the tumor, it would improve outcomes and lessen side effects.
To deliver the drugs to the tumor, the researchers bound the two therapies to a blood protein that circulates and binds to collagen in areas of vascular injury, causing blood to coagulate and seal up the injury. Because a tumor is filled with leaky blood vessels, the protein would see those vessels as vascular injury and bind to them, delivering the therapies directly into the tumor’s collagen.
The IV-administered therapy also has the advantage of finding and treating metastatic tumors throughout the body that may be unknown to the patient.
Initial results were promising. The researchers found that a combination of CPI and IL-2 administered via their technique eradicated breast tumors in 9 of 13 animal models. In contrast, when the researchers administered the drugs without the collagen-seeking protein, only one breast tumor was eradicated.
The technique also slowed the growth of melanoma and colon tumors and reduced liver and lung toxicity from the drugs, which would translate into fewer side effects for patients.
“We now may be able to create a comfortable immunotherapy for cancer patients,” Ishihara said. “One that improves both safety and efficacy.”
Bringing the therapy to patients
Next the group will work to improve efficacy even more by exploring the technique with other molecules, including molecules that were developed for cancer therapies but deemed too toxic for patients. The ultimate goal is to begin testing these combined therapies in clinical trials, ideally within three years.
“This therapy could be relevant to many solid tumors,” Hubbell said. “We want to move this forward to clinical trials and perhaps help patients who have not responded to these therapies before.”
Other authors on the paper include Stephen Kron, professor of molecular genetics and cell biology; postdoctoral fellows Ako Ishihara and Steve Seung-Young Lee; postdoctoral scientist John-Michael Williford; graduate students Laura Gray, Peyman Hosseinchi, Aslan Mansurov, Lambert Potin, Michal M. Raczy, and Koichi Sasaki; visiting scientists Kazuto Fukunaga and Kiyomitsu Katsumata; and Mariko Yasui, Hiroyuki Abe, Masashi Fukayama of the University of Tokyo.
Citation: “Targeted antibody and cytokine cancer immunotherapies through collagen affinity.” Ishihara et al. Science Translational Medicine, doi: 10.1126/scitranslmed.aau3259
Funding: European Research Commission, National Cancer Institute, and National Institute of Biomedical Imaging and Bioengineering.
—This story first appeared on the Institute for Molecular Engineering website.